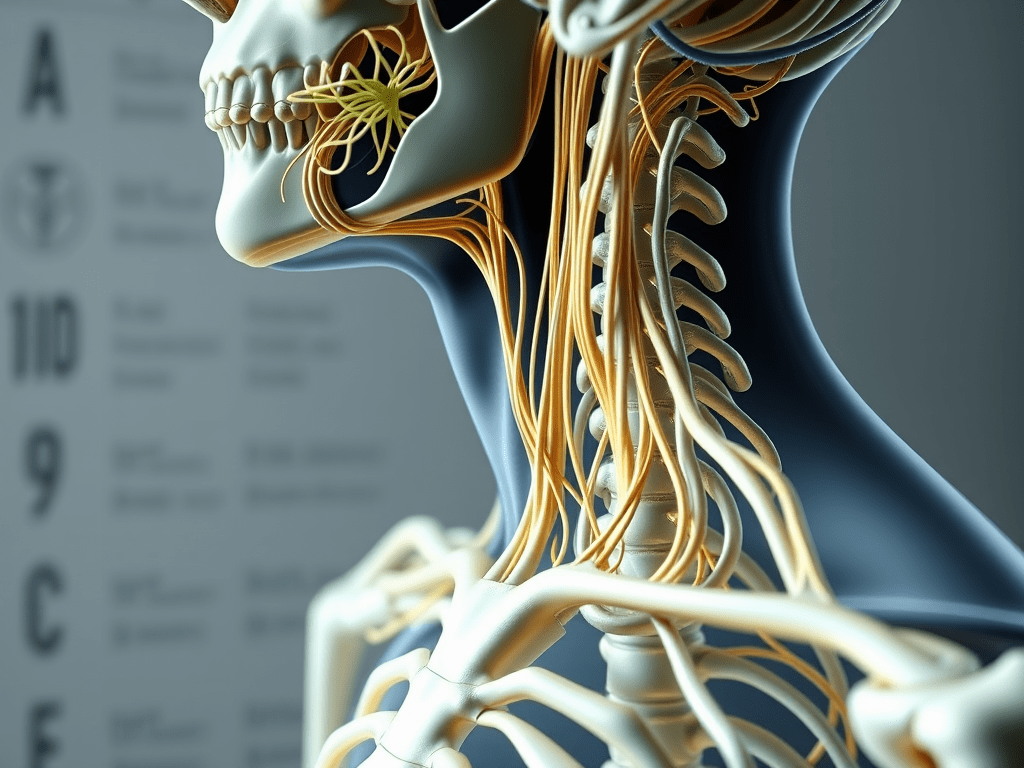
What is a Brachial Plexus Injury?
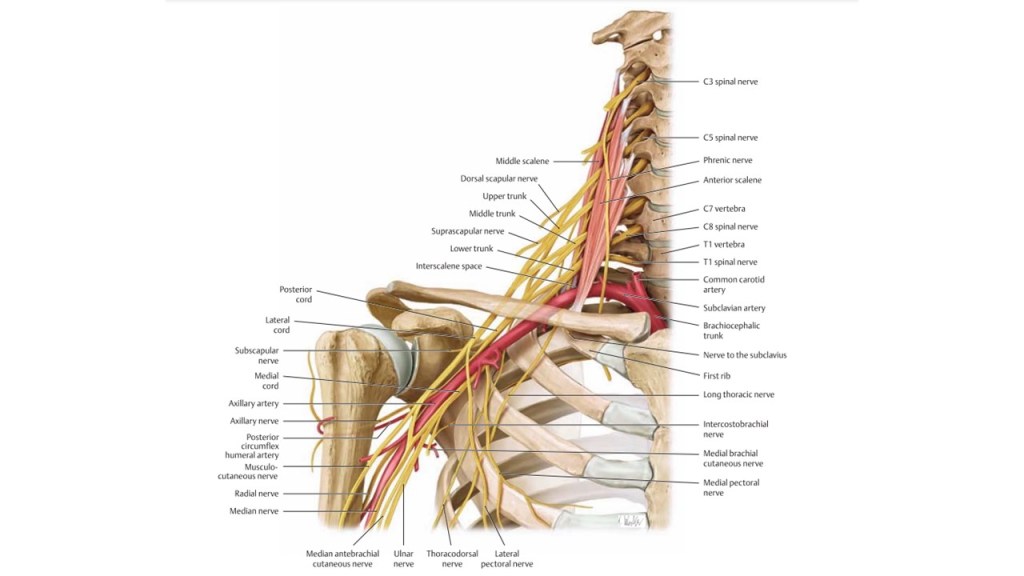
A brachial plexus injury involves damage to a network of nerves called the brachial plexus, which originates from the spinal cord in the neck region (C5-T1 vertebrae). These nerves control movements and sensations in the shoulder, arm, and hand.
Causes of Brachial Plexus Injuries
- Traffic accidents (most common in Thailand)
- Falls or high-impact injuries to the neck or shoulder
- Open wounds, such as knife cuts or gunshot injuries
Symptoms of a Brachial Plexus Injury

Symptoms depend on the severity and location of the injury:
- Upper Brachial Plexus Injury (C5, C6)
- Weakness in shoulder and elbow movement
- Loss of sensation in the shoulder and upper arm
- Difficulty lifting the arm or bending the elbow
- Lower Brachial Plexus Injury (C8, T1)
- Weakness in hand and wrist movements
- Numbness or tingling in the hand or fingers
- Panplexus Injuries
- Weakness or paralysis of the entire arm
- Loss of sensation from the shoulder to the hand
- Severe nerve pain (burning, shooting, or sharp pain)
How is the Injury Diagnosed?
Your doctor may recommend:
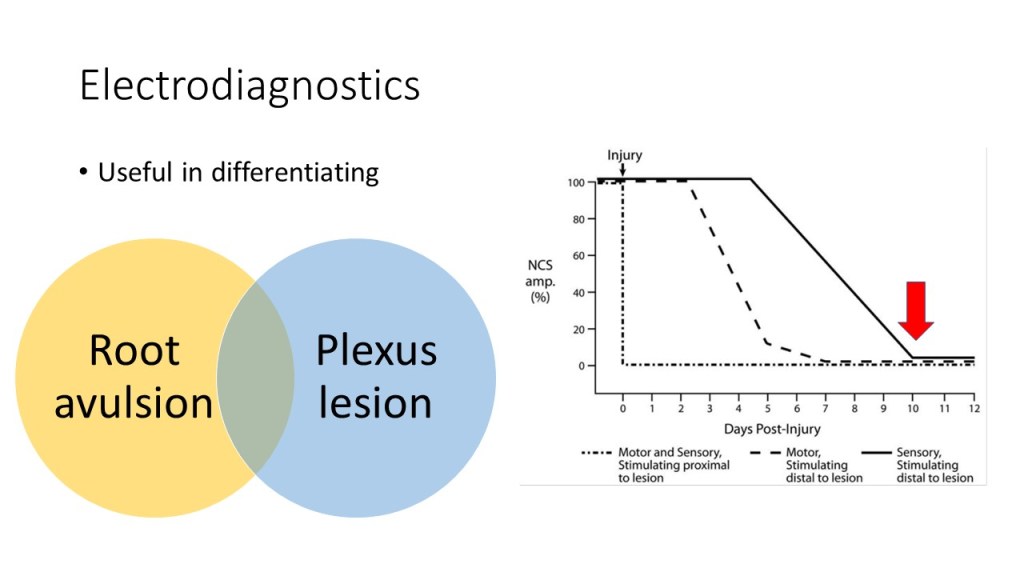
- Physical examination: To assess muscle strength, sensation, and overall nerve function.
- MRI scans of cervical spine and brachial plexus: To check for nerve damage or tears (avulsion).
- Nerve and muscle tests (EMG/NCS): To confirm the severity and location of the injury.

Treatment Options
- Mild Injuries
- Often recover naturally with physical therapy.
- Surgery is not usually required.
- Severe Injuries
- May require surgery if nerves cannot recover on their own.
- Open wound injuries (knife or sharp objects): Surgery within 72 hours.
- Blunt trauma or unclear nerve damage: Surgery after 4–6 weeks or longer.
- Nerve root avulsion: Surgery typically within 2–6 months.


Surgical Treatment of Brachial Plexus Injuries: What Are the Procedures?
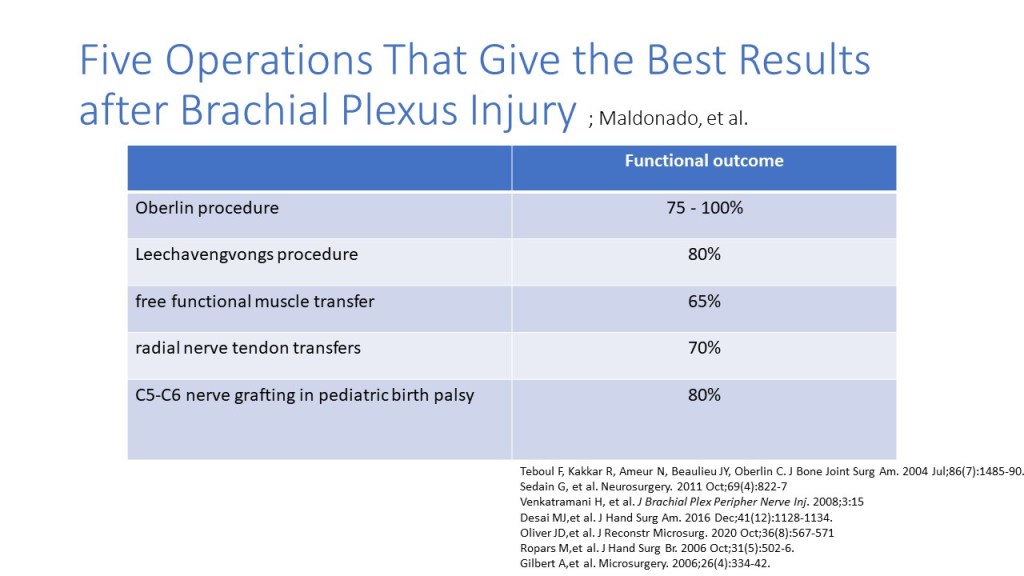
Choosing the Surgical Approach
The choice of surgical method depends on the surgeon’s discretion. Each patient’s injury is unique, differing in location, severity, and the nerves available for repair. There is no universal standard surgical procedure, and the approach varies for each individual.
Primary Goals of Recovery
- The most critical function to restore is the ability to bend the elbow.
- This is followed by restoring shoulder abduction and elevation.
- Hand function recovery, including gripping, opening the hand, and fine motor skills, is particularly challenging. In cases of severe injury with complete loss of nerve function in the arm, restoring hand function is almost impossible.

Surgical Options
- Neurolysis (Scar Tissue Removal): To release pressure on the nerves.
- Neurolysis and Direct Nerve Repair: Damaged nerve segments with scars are removed and the remaining nerve stumps are directly sutured.
- Nerve Grafting: If the scarred segment is too long for direct repair, a nerve graft may be used to bridge the gap. Sensory nerves from other areas, such as the foot, are commonly used.
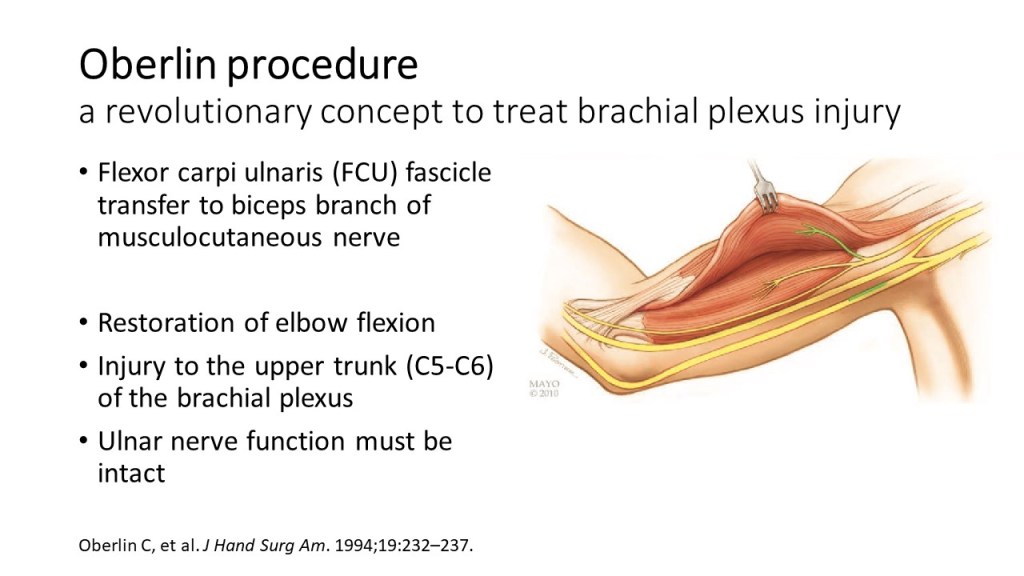
- Nerve Transfer: A healthy, functioning nerve (donor nerve) is rerouted and connected to the non-functional nerve (recipient nerve) to restore function.

Use of Donor Nerves
The outcome depends on the availability and condition of donor nerves.
- For example, if a patient loses elbow flexion but retains normal hand function, part of the nerve controlling wrist flexion can be transferred to restore elbow flexion (plexoplexal nerve transfer).
- In cases where all levels of the brachial plexus are damaged, no usable donor nerves may remain. In such situations, other nerves like the spinal accessory nerve (used for shoulder shrugging), the phrenic nerve (diaphragm control), or intercostal nerves (rib movement) may be used. However, outcomes from these transfers are generally less favorable compared to plexoplexal nerve transfers.

Is Surgery Always Successful?
Surgical outcomes vary and depend on the type and severity of the injury. While some procedures yield good results, others may have limited success. It is essential for patients to discuss realistic treatment goals with their doctor.
💡 Even with surgery, full functional recovery is not guaranteed.
When Will the Muscles Start Working Again?
Nerve repair does not produce immediate results.
- After surgery, nerve fibers grow at an average rate of 1 mm per day.
- Currently, there are no proven treatments, such as medications or electrical stimulation, that can accelerate nerve regeneration.
The time it takes for muscles to regain function depends on the distance between the injured nerve and the affected muscle.
- Typically, nerve and muscle recovery takes around 6 months to 2 years
Why Timing Matters
- Nerve surgery within 6 months offers the best chance for recovery.
- Delayed surgery (beyond 1 year) is less effective.
What Can You Do While Waiting?
During recovery or waiting for surgery:
- Physical Therapy
- Prevents joint stiffness.
- Pain Management
- Medications to ease nerve pain.
- Support Devices
- Braces for the shoulder or wrist to prevent dislocation.
Key Takeaways
- Early diagnosis and treatment are crucial for recovery.
- Physical therapy is essential even before and after the surgery.
- Talk to your peripheral nerve surgeon about the best treatment plan for you.
For more information, reach out at Contact Us.
อ่านบทความภาษาไทย ได้ที่นี่ครับ
Disclaimer
This fact sheet is for informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options.
The information provided here reflects general practices and may not apply to your individual health circumstances. Outcomes and risks may vary depending on your medical history, condition, and response to treatment.
If you experience any concerning symptoms or side effects following a procedure, contact your healthcare provider immediately or seek emergency medical attention.
This material is not intended to promote or endorse any specific treatment or procedure. Decisions about your healthcare should always be made in consultation with your physician, considering your unique health needs and goals.
Leave a comment